+90 533 813 89 77
info@bookingforhealth.com
Things to know about Pancreatitis
What is Pancreatitis?
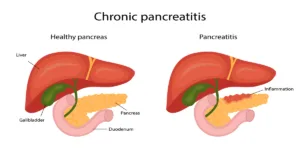
Pancreatitis is a medical condition characterized by inflammation of the pancreas. The pancreas is a vital organ responsible for producing digestive enzymes and assisting in regulating blood sugar levels. Pancreatitis is divided into two primary types: acute and chronic. Acute pancreatitis involves a sudden onset of inflammation, while chronic pancreatitis represents a long-term and recurring inflammation of the pancreas.

Symptoms of Pancreatitis
The symptoms of pancreatitis typically include severe abdominal pain, nausea, vomiting, loss of appetite, weakness, fever, and jaundice. Pain is usually felt in the upper abdomen and may radiate to the lower back.
Causes of Pancreatitis
Common causes of pancreatitis include alcohol consumption, gallstones, high triglyceride levels, overeating, or viral infections. Other factors can include trauma, medications, genetic factors, and metabolic disorders.
Differences Between Acute and Chronic Pancreatitis
Acute pancreatitis has a sudden onset, is characterized by severe pain, and often resolves with treatment. Chronic pancreatitis is a long-term condition where the pancreas undergoes permanent damage and loses its function over time.
Diagnosis and Diagnosis of Pancreatitis
Diagnosis of pancreatitis typically involves blood tests (such as amylase and lipase levels), imaging techniques (such as CT scans or ultrasound), and sometimes special procedures like endoscopic retrograde cholangiopancreatography (ERCP).
Treatment of Pancreatitis
Treatment for acute pancreatitis may require hospitalization and include measures such as fasting, intravenous fluid therapy, and pain management. Chronic pancreatitis treatment can be more complex and address consequences like diabetes or digestive issues.
Complications of Pancreatitis
If pancreatitis is left untreated or worsens, complications can arise. These complications may include pancreatic infections, pseudocysts (fluid-filled cysts), organ failure, and an increased risk of pancreatic cancer.
Relationship Between Alcohol and Pancreatitis
Alcohol consumption can increase the risk of chronic pancreatitis and exacerbate acute pancreatitis episodes. Reducing or eliminating alcohol intake is a crucial step in reducing the risk of pancreatitis.
Pancreatitis and Diabetes
Chronic pancreatitis can impact insulin production by the pancreas, potentially leading to an increased risk of diabetes. Proper management of diabetes, which may involve insulin or oral antidiabetic medications, is essential.
Pancreatitis and Nutrition
A recommended diet for pancreatitis patients can help alleviate symptoms. Initially, fasting may be necessary, followed by transitioning to a specific dietary plan. Lean proteins and easily digestible foods are often recommended.
Pancreatic Infections and Inflammatory Pancreatic Cancer
Chronic pancreatitis can increase the risk of infections due to long-term inflammation. Additionally, it is associated with a higher risk of pancreatic cancer. Therefore, regular follow-up and, if necessary, screening tests are essential.
Quality of Life After Pancreatitis
Factors affecting the quality of life after pancreatitis may include nutrition, alcohol consumption, smoking cessation, and regular medical check-ups. Paying attention to these factors can help manage the disease effectively.
Prevention of Pancreatitis
To reduce the risk of pancreatitis, it is essential to limit alcohol consumption, adopt a healthy lifestyle (including a balanced diet and exercise), control high triglyceride levels, and manage risk factors effectively.
Can Pancreatitis Be Life-Threatening?
Yes, pancreatitis can be life-threatening, especially in severe cases. Complications such as pancreatic infection, organ failure, and systemic inflammation can pose significant risks to a person’s life if not treated promptly.
Is Pancreatitis Contagious?
No, pancreatitis is not contagious. It is an inflammatory condition of the pancreas caused by various factors such as alcohol consumption, gallstones, or metabolic disorders. It cannot be spread from person to person.
How is Chronic Pancreatitis Managed Long-Term?
Managing chronic pancreatitis typically involves lifestyle modifications, including avoiding alcohol and following a low-fat diet. Pancreatic enzyme replacement therapy may be necessary to aid digestion, and careful monitoring of blood sugar levels is crucial if diabetes develops.
Can Pancreatitis Recur After Successful Treatment?
Yes, pancreatitis can recur, especially in cases of chronic pancreatitis. Even after successful treatment, ongoing medical supervision and lifestyle changes are essential to minimize the risk of recurrence.
Are There Any Complications Associated with Pancreatitis Treatment?
Treatment for pancreatitis can have complications, especially if surgical intervention is required. Potential complications include bleeding, infection, and adverse reactions to medications or procedures. These risks should be discussed with a healthcare provider.
How Can I Prevent Pancreatitis?
To prevent pancreatitis, it’s crucial to limit alcohol consumption, maintain a healthy weight, manage any underlying conditions like high triglycerides, and avoid overeating. If you have gallstones, discussing their management with a healthcare provider is essential.
Does Pancreatitis Always Lead to Diabetes?
No, pancreatitis does not always lead to diabetes. While chronic pancreatitis increases the risk of diabetes due to pancreatic damage, not all individuals with pancreatitis develop diabetes. Regular monitoring is necessary for early detection and management if it occurs.